Blue Advantage® Part B Provider-Administered Drugs Precertification Program
Effective August 1, 2023, Part B provider-administered drug precertification is required for your Blue Advantage® patients. Precertification will be managed by Prime Therapeutics.
Precertification is required for the drugs on the Blue Advantage Part B Provider-Administered Precertification Drug List when administered in a provider’s office, outpatient facility or home health setting.
Note: Gene therapy/cellular immunotherapy drugs indicated on the drug list require precertification in all places of treatment.
Patients receiving medication on the precertification drug list prior to August 1, 2023, have an authorization in our system through December 31, 2023, for continued claims payment. On January 1, 2024, continued coverage will require valid precertification through Prime Therapeutics.
You can submit precertification requests to Prime Therapeutics through the existing Pre-Service Review process:
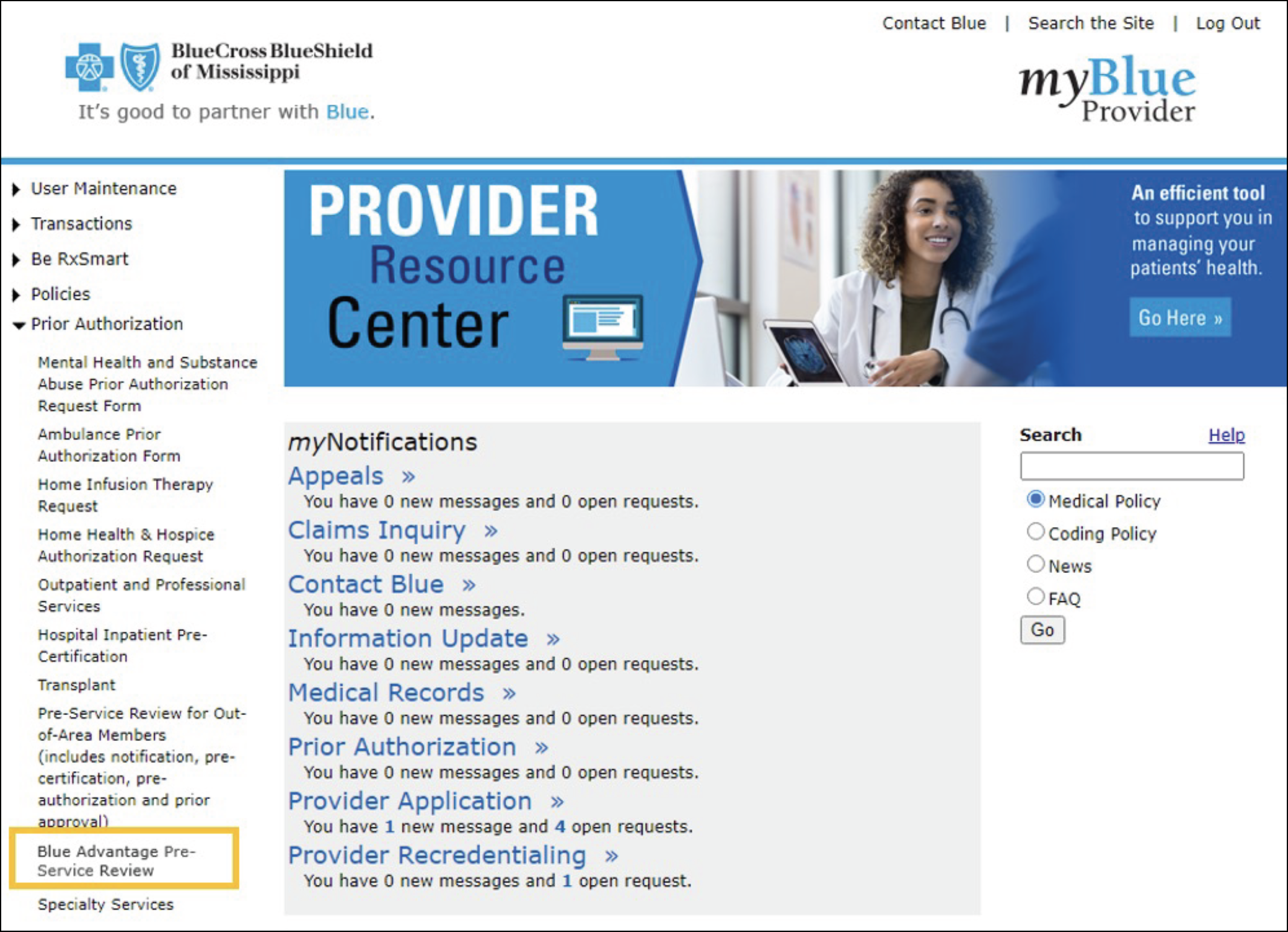
- Log in to myBlue Provider and select Blue Advantage Pre-Service Review under the Prior Authorization menu on the left side.
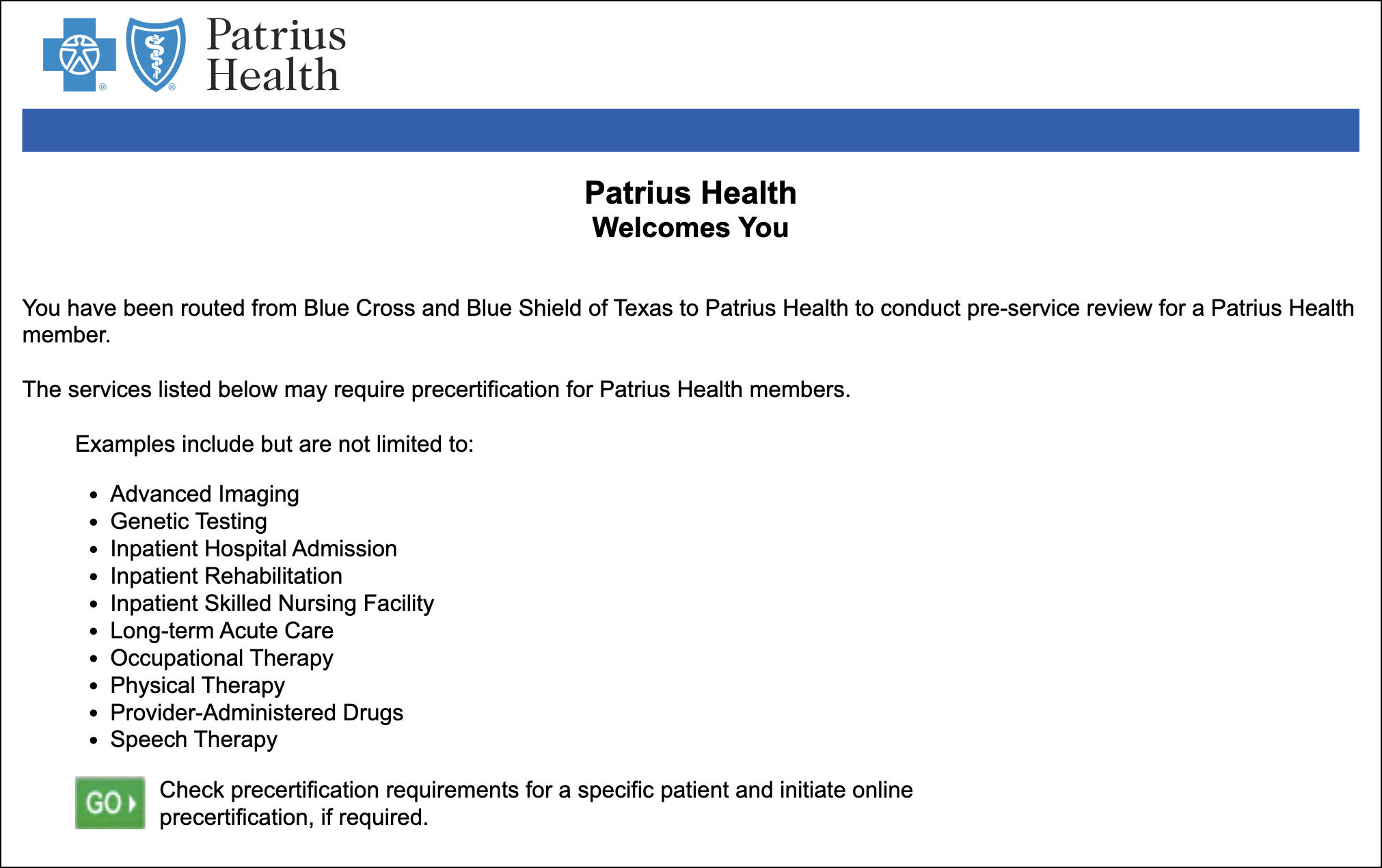
- Next, click the GO button to initiate the precertification process.
Urgent precertification requests can be submitted by contacting Prime Therapeutics at 1-800-424-8270.
Refer to our Pre-Service Review Guide as well as our Part B Provider-Administered Drug Precertification Provider Training Guide for details.
Our medical and drug policies can be found by logging in to myBlue Provider and clicking on Blue Advantage Resources.
Blue Advantage Part B Drug Step Therapy Program
Effective January 1, 2026, certain drugs in the Part B Drug Step Therapy Program are changing from non-preferred to preferred status*. Review the list below to determine which drugs require precertification or are subject to step therapy (i.e., they will be approved with a valid prescription) for your Blue Advantage patients.
| Preferred Products (No Step Therapy Required) |
Non-Preferred Products (Requires Step Therapy) | |
|---|---|---|
|
Rituximab |
|
|
| Trastuzumab |
|
|
| Bevacizumab |
|
|
Blue Advantage® PPO is provided by Blue Cross and Blue Shield of Alabama, an independent licensee of the Blue Cross and Blue Shield Association.
Prime Therapeutics® LLC, is an independent company contracted by Blue Cross and Blue Shield of Alabama to provide pharmacy benefit management services.
